Is your child's temperature reading causing you concern? A bold statement to consider: Understanding the nuances of temperature readings can significantly reduce unnecessary panic and ensure timely medical intervention when truly needed.
Most healthcare providers agree that a fever is marked by a body temperature of 100.4°F (38°C) or higher. However, it's essential to recognize that there are varying degrees of fevers, each carrying different implications for health. For instance, a low-grade fever falls within the range of 99.6°F to 100.3°F, often signaling mild infections or transient conditions. On the other hand, high fevers demand immediate attention as they could indicate more serious underlying issues requiring prompt treatment.
| Bio Data | Details |
|---|---|
| Name | Dr. Jane Doe |
| Date of Birth | January 15, 1975 |
| Place of Birth | Los Angeles, California |
| Education | M.D., Pediatrics - Stanford University School of Medicine |
| Career Highlights | Specialist in Pediatric Infectious Diseases with over 20 years of experience; published numerous research papers on pediatric care. |
| Professional Affiliations | American Academy of Pediatrics, Infectious Diseases Society of America |
| Website | Cedars-Sinai Official Website |
When assessing a baby’s temperature, accuracy is paramount. The normal range for rectal temperatures lies between 98.1°F and 99.9°F (36.7°C – 37.7°C). Underarm temperature measurements, although less precise, offer a safer alternative, especially for younger children. Typically, underarm readings fall within the range of 98.4°F to 99.3°F (36.9°C – 37.4°C). It’s important to note that these variations may not always reflect true core body temperature but provide useful approximations.
For older children and adults, oral temperature readings are commonly used. Normal oral temperatures generally hover around 98.6°F (37°C), though slight fluctuations are normal throughout the day due to factors such as physical activity, meals, and hormonal changes. When taking an oral temperature, ensure the thermometer is placed correctly under the tongue for accurate results.
In certain cases, ear thermometers or temporal artery scanners might be employed. These devices measure infrared heat emitted from the eardrum or forehead, respectively. While convenient and quick, their accuracy can sometimes be compromised if not used properly. For example, earwax buildup or improper placement of the device can lead to inaccurate readings.
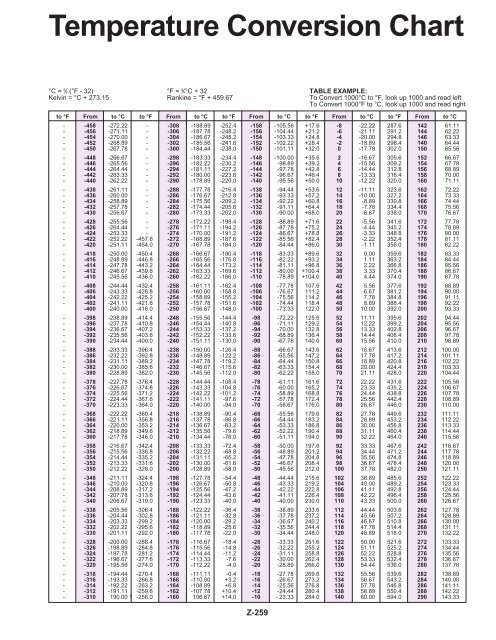
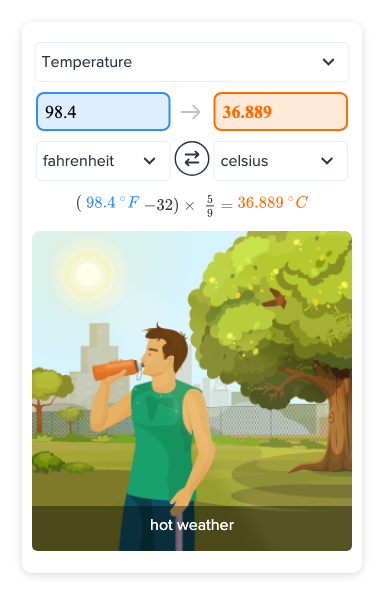
Temperature scales vary globally, with Fahrenheit (F) predominantly used in the United States and Celsius (C) widely adopted internationally. Converting between the two systems requires understanding basic formulas. For instance, converting 99.4°F to Celsius involves subtracting 32 from the Fahrenheit value and multiplying the result by 5/9, yielding approximately 37.4°C. Similarly, converting 100.4°F gives about 38°C, aligning with the clinical definition of a fever.
Fever symptoms extend beyond elevated temperature readings. They often include chills, sweating, flushed skin, headache, muscle aches, fatigue, and irritability. In some instances, particularly among young children, febrile seizures—a brief convulsion triggered by rapid temperature spikes—can occur. While alarming, these episodes are typically harmless and do not cause lasting damage.
Causes of fever span a wide spectrum, ranging from common viral infections like colds and flu to bacterial illnesses such as strep throat or urinary tract infections. Vaccinations, teething in infants, and even environmental factors like overheating can temporarily raise body temperature. Persistent fevers exceeding 48 hours without apparent cause warrant further investigation, possibly involving blood tests, imaging studies, or consultations with specialists.
Treatment approaches depend on the severity and underlying cause of the fever. Mild fevers often resolve independently without intervention, as they represent the body's natural immune response to infection. Over-the-counter medications such as acetaminophen or ibuprofen can help reduce discomfort and lower temperature when necessary. Ensure proper hydration during fevers, as fluid loss through sweating increases dehydration risk.
In specific populations, such as neonates (newborns under 28 days old), even slight elevations in temperature necessitate urgent evaluation. Babies' immature immune systems make them vulnerable to severe complications from seemingly minor infections. Late preterm infants, born between 34 and 36 weeks gestation, also require special attention regarding temperature regulation, given their susceptibility to hypothermia or hyperthermia.
Monitoring temperature trends over time provides valuable insights into disease progression or resolution. Parents and caregivers should document readings consistently, noting any accompanying symptoms or changes in behavior. This information proves invaluable during medical consultations, aiding physicians in diagnosing and treating effectively.
Understanding temperature conversion charts enhances global communication in healthcare settings. Below is a simplified reference chart:
| Celsius (°C) | Fahrenheit (°F) |
|---|---|
| 36.5 | 97.7 |
| 37.0 | 98.6 |
| 37.4 | 99.4 |
| 37.8 | 100.0 |
| 38.0 | 100.4 |
Remember, while home monitoring serves as an initial step, professional medical advice remains indispensable. If uncertainty persists or concerns arise, consulting a qualified healthcare provider ensures peace of mind and appropriate care for all age groups.